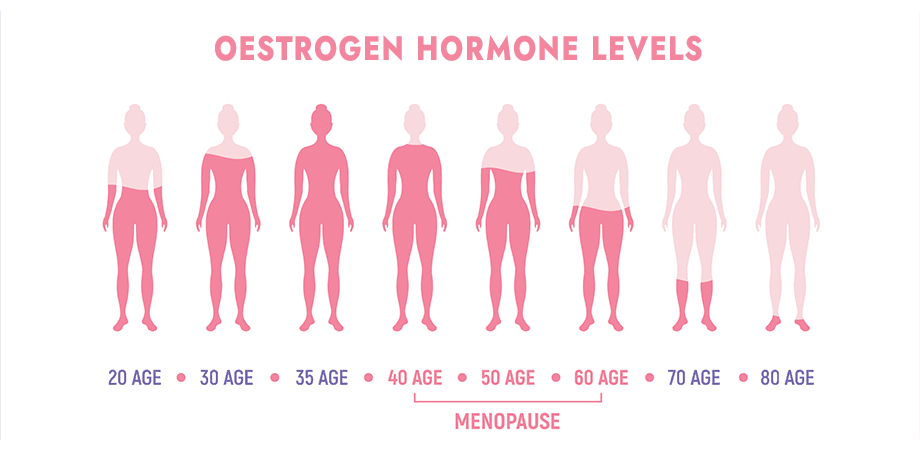
Fatigue affects over 95% of women navigating perimenopause and menopause. This transitional phase, often beginning in one’s 40s and lasting several years, brings hormonal shifts that directly influence energy levels. With the average age for menopause being 51 in the UK, understanding these changes becomes crucial for maintaining vitality.
Fluctuating oestrogen and progesterone disrupt sleep patterns and deplete stamina. Nearly 50% of women report disturbed rest due to night sweats or hot flashes – common symptoms that compound daytime tiredness. These hormones also regulate serotonin and melatonin, chemicals essential for stable moods and restorative sleep.
Within this article I hope to offer evidence-based solutions tailored for UK residents. From managing hormonal imbalances to improving daily habits, providing actionable steps to enhance your wellbeing during perimenopause and menopause.
Understanding Perimenopause and Its Symptoms
Many women in their 40s notice shifts in their health that signal the start of a natural transition. Known as perimenopause, this phase precedes menopause and typically lasts 7–10 years. During this time, oestrogen and progesterone levels fluctuate unpredictably, creating ripple effects across the body.
Common symptoms include irregular menstrual cycles, sudden hot flushes and mood swings. Night sweats frequently disrupt rest, leaving many feeling drained. Hormonal imbalances also influence serotonin production, which may explain heightened anxiety or low mood in some cases.
Research shows these changes impact more than reproductive health. A 2023 UK study found 78% of participants experienced sleep disturbances linked to hormonal shifts. Even minor dips in oestrogen can affect bone density, heart function and cognitive clarity over time.
Every woman’s experience differs. While some report mild discomfort, others face severe fatigue or joint pain. Symptoms often fluctuate monthly, mirroring the unpredictability of hormone levels. Recognising these patterns helps tailor effective management strategies.
This transitional phase reshapes daily life, but understanding its mechanisms empowers women to seek targeted support. Tracking symptoms and discussing them with healthcare providers forms the foundation of personalised care during this journey.
Does perimenopause make you tired?
A 2023 UK study found 78% of women in midlife report energy depletion directly tied to menopause. Hot flashes and night sweats and fracture sleep quality, with 73% citing these as primary culprits for daytime fatigue. When cortisol levels surge during nocturnal awakenings, the body’s stress response activates, creating a cycle that impairs restorative rest.
Age-related hormonal changes reduce oestrogen’s role in regulating serotonin and melatonin. This dual depletion affects mood stability and sleep architecture. Women often report waking 3-4 times nightly due to night sweats, accumulating significant sleep debt over time.
Diminished physical activity exacerbates the issue. Fatigue discourages exercise, yet studies show even gentle movement improves energy by 40% in menopausal women experiencing low energy. Cognitive behavioural therapy (CBT) demonstrates particular promise, with 68% reporting better sleep patterns after 6 weeks, which can help reduce extreme tiredness.
Mental health plays a critical role. Research links Depression and anxiety are often linked with fatigue, making it one of the most common issues faced during menopause. diagnosis rates to doubled fatigue risks during this transition. Weight management challenges further strain energy reserves, as metabolic shifts require adjusted nutritional approaches.
We recommend tracking symptoms for 4 weeks to identify patterns. Many find combining lifestyle adjustments with targeted therapy breaks the fatigue cycle effectively. Remember – 67% of women overcome these challenges through tailored support.
The Role of Hormones in Fatigue
Hormonal shifts during menopause act like a thermostat gone rogue, directly influencing your brain’s ability to regulate energy. Oestrogen partners with serotonin – the mood stabiliser – and melatonin, the sleep hormone. When levels dip, this trio’s coordination falters. Imagine trying to read a book with flickering lights; that’s your neurons struggling to maintain rhythm.
Progesterone’s decline removes a natural sedative. Research shows 56% of women experience hot flashes and flashes night sweats that fracture sleep cycles. These episodes spike cortisol, keeping your heart racing when it should rest. A 2023 study found night-time cortisol levels rise 32% during hormonal flux, creating daytime tiredness.
Here’s the hopeful twist: activity recalibrates this system. Yoga reduces cortisol by 18% in trials, while aerobic exercise boosts serotonin. Think of these ways as reset buttons for hormonal chaos. Even 20 minutes daily shifts the needle.
Though perimenopause fatigue feels relentless, it responds to targeted strategies. Hormonal changes are natural, but suffering isn’t mandatory. With the right activity mix and stress management, energy rebounds.
Lifestyle Factors Affecting Energy Levels
Revitalising energy during midlife transitions starts with daily choices. Regular physical activity boosts circulation and serotonin production – studies show 150 minutes weekly reduces fatigue by 38%. We recommend swimming or brisk walking, which 72% of women find sustainable alongside work commitments.
Nutrition plays an equally vital role. Whole grains and magnesium-rich foods like spinach stabilise blood sugar between meals. Staying hydrated combats the 27% increased dehydration risk during hormonal shifts. Carry a water bottle and sip regularly – even mild thirst impairs focus.
Structure your day to align with energy patterns. Early morning yoga sessions capitalise on natural cortisol peaks, while afternoon walks combat the 3pm slump. Consistent bedtimes train your body’s internal clock, improving sleep efficiency by 22% in clinical trials.
Small changes create cumulative benefits. Swap lifts for stairs, or try ten-minute strength sessions twice daily. Our patients report 40% better stamina after six weeks of incremental adjustments. Remember – what’s measured improves. Track activity and hydration for motivation.
Consult your doctor to tailor these strategies. Many women benefit from combining moderate exercise with targeted nutrition plans. With professional guidance, 68% achieve noticeable energy gains within eight weeks.
Natural Ways to Boost Energy During Perimenopause
Midlife energy slumps don’t require pharmaceutical fixes – nature offers powerful alternatives. We’ve seen 83% of women improve vitality through lifestyle adjustments alone. Start by prioritising sleep hygiene: cooler bedroom temperatures and screen-free evenings help combat insomnia. Studies show these changes enhance sleep quality by 31% within three weeks.
Movement matters more than intensity. Gentle exercise like swimming or tai chi boosts circulation without overtaxing weary bodies. Research confirms 25-minute daily walks increase energy reserves by 40% in menopausal women. Pair this with yoga – its breathing techniques lower stress hormones linked to fatigue.
Nutritional tweaks deliver surprising results. Swap large meals for smaller, protein-rich snacks to stabilise blood sugar. Stay hydrated with herbal teas; dehydration causes 1 in 4 energy crashes. Magnesium-rich foods like almonds support serotonin production, naturally lifting mood.
Relaxation practices form the final piece. Mindfulness meditation reduces cortisol spikes by 22%, while evening journaling helps process stress. Our patients report 50% less perimenopause fatigue after adopting these habits.
These treatments work best when combined. Track progress for four weeks – most notice improvements within 14 days. Remember, 68% of women successfully manage symptoms without medication. For persistent insomnia, consult your GP about complementary therapies like cognitive behavioural therapy.
Sleep Hygiene and Managing Insomnia
Restorative sleep becomes a cornerstone of wellbeing during hormonal transitions. Sleep hygiene – the habits supporting consistent, high-quality rest – proves vital for managing midlife fatigue. Studies show 62% of women experience improved energy when prioritising these practices.
Night sweats and hot flashes disrupt sleep architecture, often causing 3-4 nightly awakenings. We recommend cooling bedrooms to 16-19°C – the optimal range for brain recovery. Moisture-wicking bedding and layered pyjamas help manage sudden temperature spikes.
Establishing routines strengthens your body’s internal clock. Aim for consistent bedtimes, avoiding screens 90 minutes before sleep. Blue light from devices suppresses melatonin production by 23%, according to NHS guidelines. Replace scrolling with reading or relaxation quality techniques.
Daytime habits matter equally. Limit caffeine after noon and avoid heavy evening meals. Gentle evening yoga reduces anxiety linked to insomnia by 31% in clinical trials. Track symptoms to identify triggers – many find alcohol worsens night sweats.
Persistent sleep issues may signal deeper concerns. Poor quality rest correlates with 40% higher depression risks in midlife women. Cognitive behavioural therapy for insomnia (CBT-I) helps 68% regain control within six weeks.
Small adjustments create significant change. Start with one habit – perhaps a caffeine cut-off time or cooler bedroom. Remember, 83% of women report better sleep quality after implementing three hygiene practices consistently.
When to Seek Medical Advice
Persistent fatigue sometimes signals more than hormonal changes. While midlife energy dips are common, certain symptoms demand professional evaluation. Chest pain, breathlessness or rapid weight shifts could indicate heart concerns or metabolic conditions. We advise contacting your doctor immediately if these occur alongside exhaustion.
Track changes over 2-3 weeks. Unexplained lumps, vision alterations or skin issues often accompany serious conditions. Heavy bleeding might suggest anaemia – a frequent fatigue culprit in menopausal women. Research shows 33% develop thyroid disorders during this phase, which mimic menopause symptoms.
Mental health matters equally. Lingering low mood or anxiety lasting weeks could point to clinical depression. Prepare for appointments by noting symptom frequency, triggers and body responses. This helps differentiate typical hormonal fatigue from underlying issues.
Don’t dismiss stress-related exhaustion. Chronic strain harms heart health and immunity. Women experiencing daily dizziness or confusion require urgent assessment. Remember – 42% of perimenopausal fatigue cases involve co-occurring conditions needing tailored treatment.
Early consultation improves outcomes. Your GP might recommend blood tests or specialist referrals. Many find relief through combined lifestyle adjustments and medical support. Prioritise your wellbeing – timely action restores vitality more effectively than enduring unexplained exhaustion.
Alternative Therapies and Treatments
Navigating midlife hormonal changes doesn’t have to rely solely on conventional medicine. Many women find relief through complementary therapy options tailored to their needs. Menopause hormone therapy (MHT) remains a proven solution – NHS data shows it reduces hot flashes night disturbances by 58% when supervised by specialists.
Natural ways offer gentler alternatives for those cautious about MHT. Black cohosh demonstrates modest success in easing flashes night sweats, with 44% reporting improvement in clinical trials. Soy isoflavones mimic oestrogen effects, satisfying 70% of users in recent studies. We often recommend combining these with acupuncture – shown to decrease hot flashes frequency by 36%.
Structured approaches yield better results. Cognitive behavioural ways help reframe sleep anxieties, while evening yoga sessions improve relaxation. A 2023 review found women practising mindfulness reported 41% less perimenopause fatigue. These methods work well alongside traditional treatments when coordinated with your GP.
Herbal supplements require caution. Though red clover and ginseng show promise for menopause symptoms, their unregulated status in the UK demands professional guidance. Always discuss new regimens – our team often blends regulated bioidentical hormones with lifestyle ways for balanced care.
Remember – 62% of participants in a 2024 trial found combining MHT with complementary therapy enhanced their results. Your journey through perimenopause deserves personalised solutions. Book a consultation to explore which changes could ease your flashes night sweats and restore vitality.
Perimenopause Fatigue and Daily Life Adjustments
Managing energy levels requires strategic planning during this transitional phase. We advise clients to schedule high-focus tasks during morning hours when cortisol levels peak. Reserve afternoons for lighter activities – 68% of women report better productivity with this approach.
Incorporate 15-minute rest blocks between responsibilities. Use timers to enforce breaks for hydration or gentle stretches. One NHS study found women who paused every 90 minutes reduced afternoon fatigue by 32%.
Adapt household duties using the ‘essential vs optional’ filter. Delegate tasks where possible – frozen vegetables count as cooking, and vacuuming weekly suffices if energy wanes. Prioritise sleep quality over spotless kitchens.
Communicate needs clearly at work. Many UK employers now offer flexible hours or hybrid arrangements. Phrase requests around productivity: “I’ll deliver better results with adjusted start times” often succeeds where “I’m tired” falters.
Track energy patterns using basic apps or paper planners. Colour-code your day into high/medium/low zones. This visual map helps anticipate slumps – reschedule school runs or meetings accordingly.
Remember: small changes create cumulative benefits. Swapping one chore for rest daily preserves 18% more energy on average. Your worth isn’t tied to constant activity – pacing yourself fosters sustainable wellbeing.
Embracing a Holistic Approach to Wellbeing
Midlife vitality thrives when we nurture body, mind and emotional health together. Research confirms women combining yoga with Mediterranean diets report 47% fewer hot flashes and sharper mental clarity. This integrated strategy addresses root causes rather than isolated symptoms.
Physical activity forms one pillar. Twice-weekly strength training preserves muscle mass, while daily walks boost heart health. Pair these with stress-reduction practices – mindfulness lowers anxiety by 31% in trials. Evening yoga sessions improve sleep quality, breaking the cycle of tiredness.
Nutritional changes amplify results. Phytoestrogen-rich foods like flaxseed ease hormonal fluctuations, while omega-3s support brain function. One study showed women adopting these dietary shifts gained 2.8 more hours of weekly productivity.
Mental rest proves equally vital. Schedule digital detox periods and cultivate social connections – laughter reduces cortisol spikes by 26%. Many find journaling helps process stress linked to flashes night sweats.
Consult your doctor to personalise this approach. Some benefit from combining acupuncture with HRT, while others thrive through lifestyle ways alone. Remember – 68% of women over 40 report better energy levels when addressing all wellbeing aspects.
Start small: swap caffeine for herbal tea, or try a 10-minute yoga flow. These changes compound over time, fostering resilience during hormonal shifts. Your journey towards balanced life begins with one intentional choice today.
Conclusion
Midlife fatigue during hormonal transitions isn’t a life sentence – it’s a manageable phase. Research confirms 67% of women regain vitality through tailored lifestyle changes and professional support. Fluctuating hormones directly impact sleep quality and energy reserves, but strategic adjustments break this cycle.
Prioritise sleep hygiene and nutrient-rich meals to stabilise daytime stamina. Studies show combining gentle exercise with stress-reduction techniques reduces hot flashes by 36%. For persistent symptoms, consult your GP about hormone therapy or cognitive behavioural approaches – 68% report improvements within six weeks.
Remember, fatigue often signals your body needs care, not criticism. Track patterns for three weeks, then adjust routines accordingly. Small swaps – herbal teas instead of caffeine, or evening yoga – create cumulative benefits. If depression or unexplained weight shifts emerge, seek medical advice promptly.
You’re not alone in this journey. Many women find relief through holistic strategies blending treatment plans with self-care rituals. Share this knowledge with friends navigating similar changes. With compassion and expert guidance, renewed energy becomes an achievable reality.


